How do you deliver a
Competitive Benefits Experience
without a large investment of time and money?

Leverage our Benefit Navigators, Innovative
Technology and Custom Provider Networks to deliver
the experience your clients demand.

ENROLLMENT
Outbound phone calls to employees are made by our multi-lingual benefit navigation team to answer questions and confirm coverage options. We make sure employees have the information they need to make informed decisions about their health care benefits.
OUTBOUND WELCOME CALLS
It starts with Hello! At the beginning of the plan year, we make outbound phone calls to each member and open the lines of communication. Our multi-lingual team reviews the member benefits and we make sure they know that our number is all they need to get their questions answered...it’s the start of a great relationship.
A NEW LEVEL OF CUSTOMER CARE
Our goal is to eliminate all surprises in coverage by ...
- Creating access to the employee’s preferred provider
- Setting appointments and confirming benefits
- Assisting in the claims process
- Wrapping our customer care across all benefits.
UTILIZING BENEFITS
- Educating the member on the value of the programs
- Enrolling members in the programs
- Explaining how to use the services effectively
- Encouraging use through outbound call campaigns and app messaging
Data-Driven Analytics

- Uncover client and product insights
- Understand each client’s:
- Benefits utilization
- Customer satisfaction
- Drive employee behavior to increase bottom line
Go Beyond the Network

ON-DEMAND PROVIDER CONTRACTING
- Creates on-demand contracts between third party administrators and providers.
- Allows members to access virtually any provider for their services.
- Achieves 90%+ success rate in getting practices to contract with our partners.
Technology Drives Innovation
Transparent Healthcare delivers innovative technology solutions that can reduce the cost of care while improving the member experience
ID CARD
Electronic version of member ID card with real-time eligibility.
MY ACCOUNT
Member demographics, policies, and plan benefits.
ONE CLICK CONNECT
Easy access to your benefit partners.
CUSTOMER SERVICE
Multi-lingual support for all benefits through live chat or phone.

APPOINTMENT
Customer service team will make provider appointments, ensuring members stay in network.
MESSAGING
Outbound communication to employees to drive behavior and engagement.
CLAIMS
Easy real-time claims upload using camera.
Enrollment Technologies
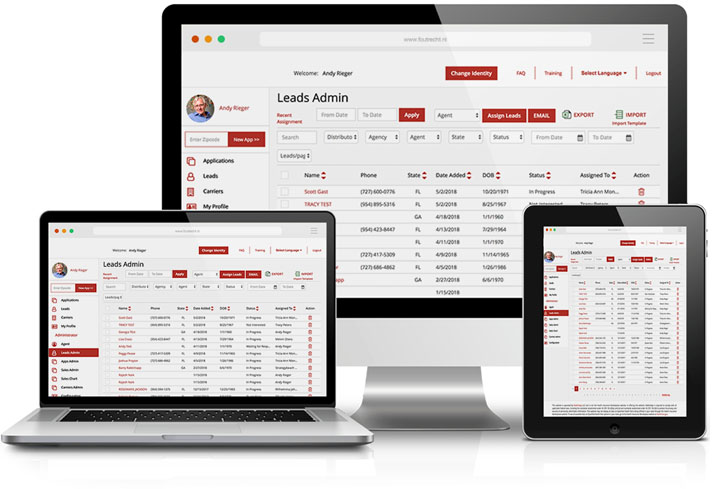
- Electronic Health Questionnaires
- Provider Nomination Forms
- Web Based Enrollment Platform